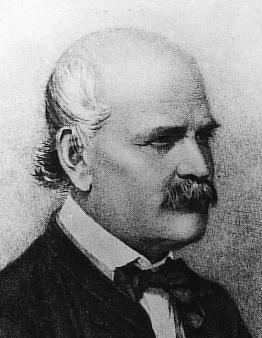
Ignaz Semmelweis is today credited with the realization in the mid-1800’s that death rates at maternity clinics could be significantly decreased if doctors simply washed their hands with chlorine wash between handling cadavers and delivering babies. For his trouble he was dismissed as a loony and beaten to death in an insane asylum, 20 years before Louis Pasteur’s germ theory of disease introduced the rest of the world to the notion of microscopic organisms that can kill you.
It wasn’t until 1928 that Alexander Fleming discovered penicillin, the first known antibacterial substance which would revolutionize medicine, earn Fleming a Nobel prize, and ultimately spawn an enormous pharmaceutical industry. Today, hand-washing and aseptic techniques are commonplace in hospitals around the world, but it was antibacterials such as penicillin and other (often synthetic) antibiotics that came to assume a prominent and ubiquitous role as the first line of defense against a plethora of potentially lethal microbes. Indeed, the effectiveness and importance of antibacterials was such that in the 1970’s surgical scrubs worn by doctors and nurses in operating theaters began to be treated with an antibacterial agent named triclosan.
Farmers also started adding antibiotics to livestock feed as a preventive measure to stop animals getting sick. However, it wasn’t long before more entrepreneurially-minded individuals woke up to the realization that there was money to be made off the general public from these substances that were thus far restricted to medicinal and veterinary contexts. Relying on the tried-and-tested sales technique of playing on the fear and ignorance of consumers, manufacturers began adding antibacterial substances (especially triclosan) to a variety of household products and marketing the resultant “antibacterial” products as important and necessary. Although this trend began slowly, the addition of antibacterials to various items grew steadily to the point where by 2001 almost 700 “antibacterial” products were available, ranging from hand cleansers and detergents to window cleaners, chopsticks and even sheets, towels, pillows and entire mattresses impregnated with antibacterial agents.
Despite what advertisers would have us believe, this sudden deluge of antibacterial agents into regular households has done little to stem the prevalence of hardy microorganisms within which human societies are constantly awash. Indeed, there is alarming and compelling evidence that saturating the environment with antibacterials and antibiotics has only increased the danger posed by disease-causing bacteria, and the medical community has recognized for some time that many of our common antibiotics are becoming increasingly ineffective.
The proximate causes of this pharmacological obsolescence can be attributed primarily to over-use of antibiotics to treat non-bacterial ailments (e.g. flu and the common cold, both of which are caused by viruses) and on the flipside, the failure of patients to complete prescribed antibiotic courses. The ultimate cause of the problem, however, is clear: it’s evolution, baby! By constantly bombarding bacteria with strong selective pressures in the form of potentially deadly antimicrobials, many bacteria have begun to evolve resistance to those substances. For example, whenever a patient fails to complete a course of antibiotics, those lucky bacteria with even mild resistance to the agent applied are able to survive and pass those resistance genes on to their progeny. Over time, and with the aid of mutation, these resistant lines of bacteria are continually selected for (i.e. leave more offspring relative to non-resistant individuals) and may ultimately evolve complete resistance to that antibacterial agent. (You can watch an animation of this process here.)
In response, humans develop different antibiotics which are then applied profligately, and to which bacteria again develop resistance. It is an evolutionary arms race, and one which we are currently losing. Part of the reason we are being outgunned is that, depending on the nature of the resistance that evolves, bacteria which become resistant to a particular antibacterial substance may simultaneously acquire resistance to a different type of antibacterial that works in a similar way, a phenomenon known as cross-resistance. (Bacteria also have another trick up their sleeve called lateral gene transfer, whereby they can acquire resistant genes from other unrelated individuals without having to inherit them from a previous generation.)
The problem is growing so acute that it seems every week brings another report from some part of the world of the spread of antibiotic-resistant “superbugs”, such as methicillin-resistant Staphylococcus aureus (MRSA). New antibiotics take substantial amounts of time (around 10-20 years) to develop and test, and as a result we are slowly but surely running out of options for combatting bacterial infection.

But what does the misuse/abuse of prescription antibiotics have to do with antibacterial chopsticks? Although the jury is still out on whether antibacterial agents added to everyday household items select for antibiotic resistance, the existing data addressing this issue are not encouraging. What is agreed on is that “antibacterial” products offer no benefit over similar non-antibacterial products. For example, “antibacterial” soap containing triclosan has been shown to be no more effective than ordinary soap in either preventing illness or reducing bacterial levels on hands. More alarmingly, laboratory studies have shown evidence for triclosan-adapted cross-resistance to antibiotics among several species of bacteria, meaning that bacteria which are exposed to triclosan and evolve resistance to it acquire resistance to other antibiotics as well. So adding triclosan to soap and then slavering it all over yourself, your bathroom, your kitchen and presumably your children is not only pointless in terms of reducing bacteria numbers, it is also potentially dangerous in the long run.
Given these dangers, we need to stop and ask ourselves this: if the evolution of antibiotic-resistant bacteria is being driven by the ubiquity of antibiotics in the modern world, is putting antibiotics into absolutely everything (and most especially things that have absolutely no need for antibiotics to begin with) really such a good idea? Although we have learned a great deal about bacteria since the time of Ignaz Semmelweiz, if we have also learned anything from evolutionary biology then that answer has to be “No”.
2 Replies to “Nobody needs antibacterial anything”